New research presented at the American College of Cardiology’s Annual Scientific Session (ACC.25) reveals that ovary removal, also known as bilateral oophorectomy, may significantly raise the risk of heart failure among women, especially when performed before natural menopause.
The study focused on 6,814 women from the National Health and Nutrition Examination Survey (NHANES), spanning 2017 to 2023. It found that women who had both ovaries removed were 1.5 times more likely to develop heart failure compared to those who retained their ovaries. Among White women or those undergoing the procedure at younger ages, the risk was nearly twofold higher.
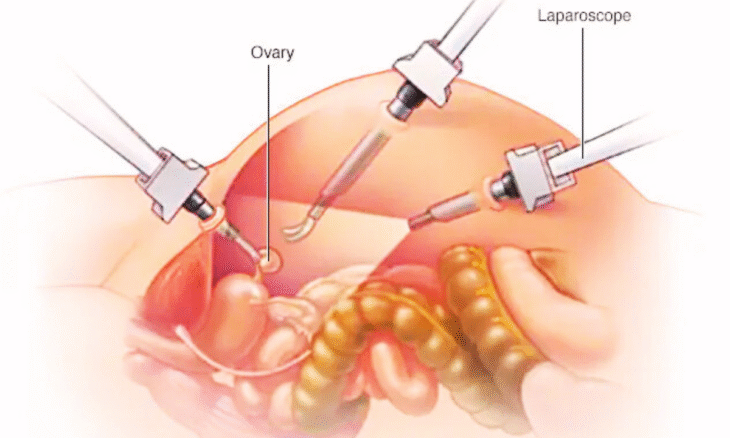
Bilateral oophorectomy is typically advised for managing or preventing conditions like ovarian cancer, endometriosis, pelvic inflammatory disease, and excessive menstrual bleeding. However, researchers found that the procedure’s hormonal effects—specifically the abrupt loss of estrogen and progesterone—may contribute to early-onset menopause, a known risk factor for cardiovascular issues.
“We believe the increased risk of heart failure stems from early menopause induced by surgery, which differs from menopause caused by natural factors,” said Dr Narathorn Kulthamrongsri, lead author and internal medicine resident at the University of Hawaii.
The average age of ovary removal among participants was 43.6 years, with heart failure diagnoses occurring around 57. Each additional year in age at the time of surgery delayed heart failure onset by about 0.6 years, the researchers found.
Risk Assessment Ovary Removal
The study urges clinicians to incorporate cardiovascular risk assessments and closer heart monitoring when advising women considering ovary removal before age 51—the typical age of natural menopause. It also raises the need for healthcare providers to discuss potential lifestyle interventions and hormone replacement therapy (HRT) to mitigate heart risks post-surgery.
Interestingly, the findings also identified racial disparities. Despite previous data indicating that Black individuals experience worse heart failure outcomes, White women showed a higher risk of heart failure following oophorectomy. Researchers attribute this to varying causes of heart disease between demographic groups and the hormonal impact on heart tissue.
While the study was limited by its reliance on self-reported data and did not assess the timing between surgery and heart failure onset, it adds to a growing body of literature indicating early surgical menopause may have long-term cardiovascular consequences.
Experts call for further large-scale studies to confirm these results and explore preventive strategies, including regular cardiovascular screening and the potential use of heart-protective medications.